AECOM M&A Change Management and Communications
Client: AECOM
Industry: Architecture, Building and Construction
Number of Employees: 50,000 employees globally
When AECOM’s U.S. workforce grew from 10,000 to 40,000 employees nationwide as a result of a merger/acquisition, they turned to Blue for assistance in introducing a new benefits program. There were significant changes for all employees, particularly affecting the medical plan options and their costs.
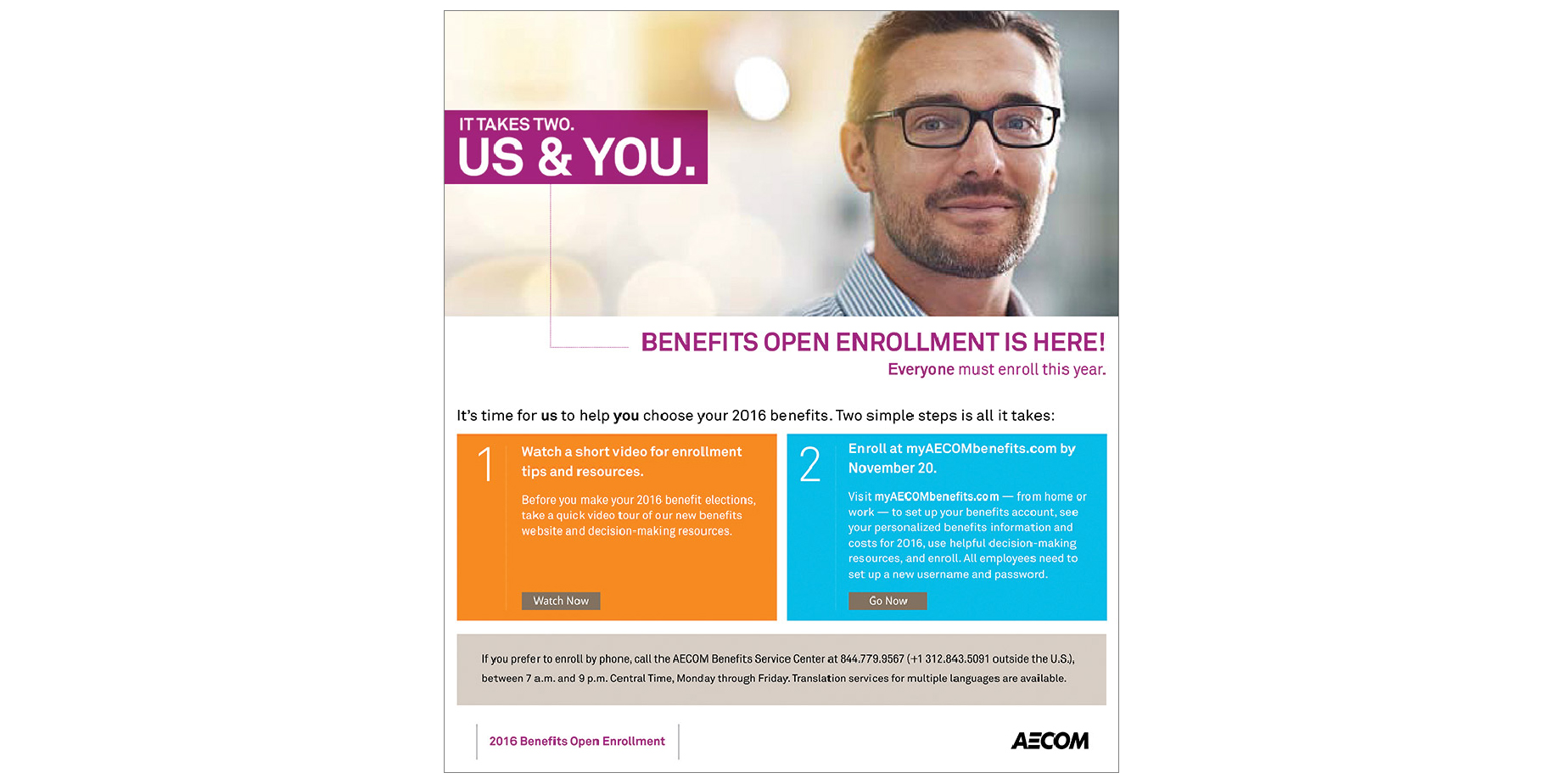
Together with AECOM’s consulting team of Towers Watson and Aon Hewitt, Blue created a successful multimedia campaign featuring a new benefits brand, It Takes Two. Us & You., that conceptually shifted the focus from the needs of the employee to the needs of the employee and the shared needs of the business. The campaign emphasized that both employees and the company have important needs and responsibilities, and must work together to manage costs, build a strong business and achieve AECOM’s ultimate goal: to deliver a better world.
The campaign delivered enrollment results that exceeded everyone’s expectations:
- HDHP enrollment increased from 68% to 81%, far surpassing management’s goal to maintain enrollment levels. And, more than half of the HDHP enrollees elected the option that provides the most overall plan value for AECOM and the majority of employees.
- More than 80% of eligible employees actively enrolled for their benefits. These numbers demonstrate that employees read the communications, understood the importance of making new choices, and wanted to make active, informed choices rather than be enrolled in default options.
- Employees took the time to learn about their new benefits: an online Health Plan Comparison tool was accessed by nearly 25,000 employees.
Due to the new benefits program, new cost sharing approach, successful plan migration results and a touch of Blue, AECOM was able to reduce their project health care cost increase by half while continuing to provide excellent family-friendly, cost-effective choices for employees and their families.